Part 2 The Pandemic Agreement: A Turning Point for Global Health Equity and Security?

After more than three years of intense negotiations, the agreement is a step forward. But does it truly advance global health equity or risk repeating past mistakes?
On May 20, 2025, history was made. The 78th World Health Assembly adopted the long-awaited Pandemic Agreement, a multilateral framework designed to guide the world in preventing, preparing for, and responding to future health emergencies. After over three years of intense negotiations and deep global reflection following COVID-19, the agreement marks an ambitious step forward. But does it truly advance global health equity or risk repeating the same mistakes?
For the second part of our two-part article series, we interacted with Melissa Scharwey from Médecins Sans Frontières (MSF), Valentina Voican from the German Federal Ministry of Health (BMG) and Dr Oliver Morgan, Director of the WHO Hub for Pandemic and Epidemic Intelligence in Berlin.
Their perspectives, grounded in policy, practice, and front-line public health, offer a deeper look into what this agreement delivers, where it still falls short, and what comes next.
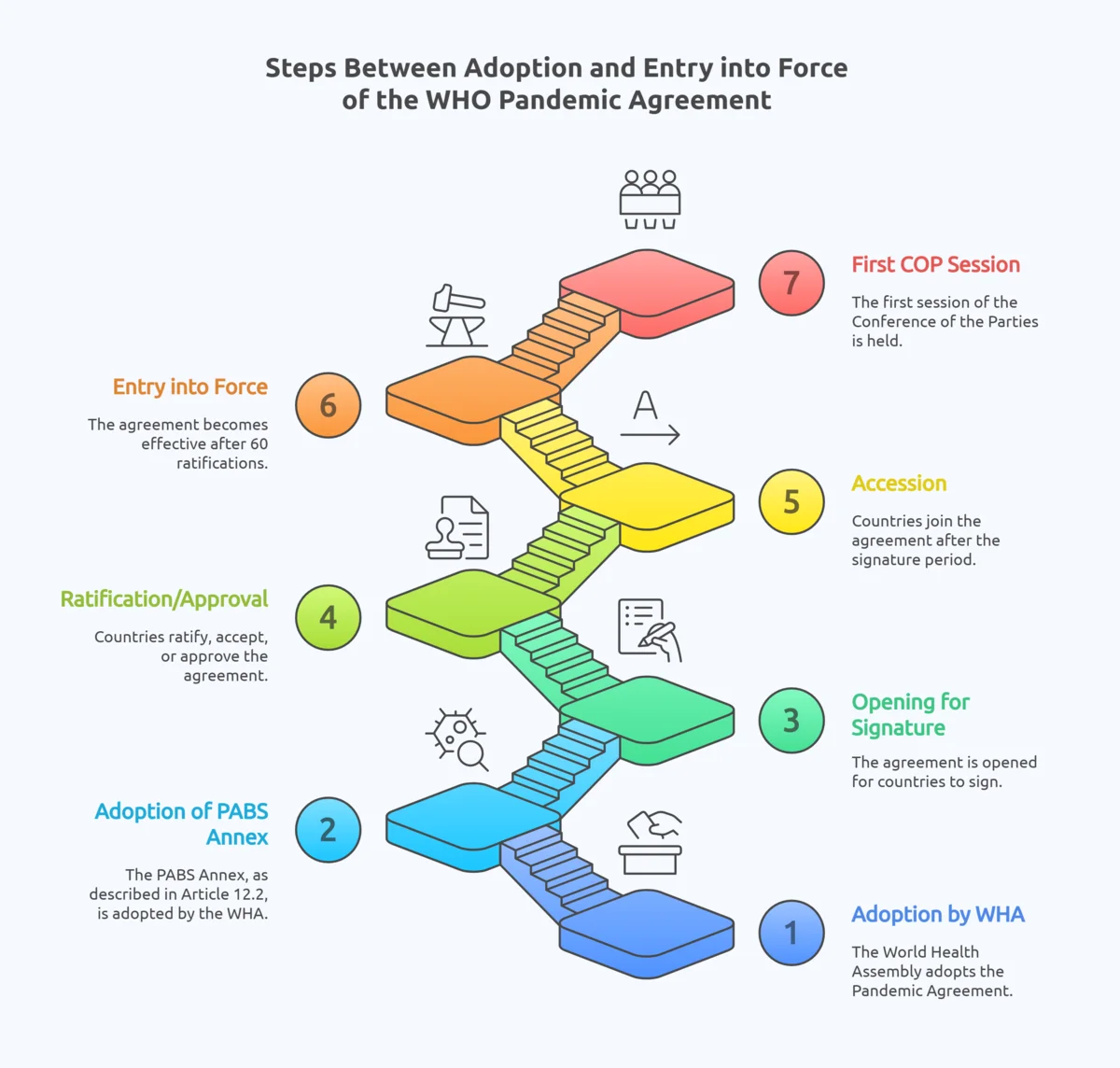
The Next Big Hurdle: PABS and Ratification
One piece is still missing: the PABS annex, which is to be negotiated over the next year. This annex will determine how pathogen samples and benefits, like vaccines or treatments are shared. The idea is simple: if countries share outbreak data, they should receive fair access to resulting medical countermeasures.
However, as Valentina from the German Federal Ministry of Health points out, "It's a very complex and technical issue.” She further emphasised that expert involvement is required to ensure the development of a functional system.
The annex is pivotal for the equity promises of the agreement. During COVID-19, data shared by low-income countries led to vaccines primarily benefiting wealthier nations. But reopening past debates may delay progress. “Bringing old discussions or things that we couldn't agree on back to the table will not help,” Valentina stresses that realistic timelines and a focus on what is feasible are essential in order to bring this process to a successful outcome.
The treaty enters into force only after 60 countries ratify it. While the goal is to finalize the PABS annex by the 79. World Health Assembly 2026, many experts say one year is not enough. “The timeline is very ambitious… but if we need more time, we should take it to reach a good result,” Valentina says. “Our goal is a system that works and can make a real difference.”
Meanwhile, the withdrawal of the U.S. from WHO during the final stages of negotiations casts a shadow over the pandemic agreement. Once the largest funder of global health and a major player in biomedical innovation, its absence could pose a threat to the agreement’s universality and future implementation, especially in areas like funding, pharmaceutical cooperation, and global coordination.
Yet as Melissa of MSF points out, implementation ultimately lies at the national level: “Each of our countries has a responsibility to implement… whether the US is doing that or not.” At the same time, she acknowledges the “massive gap” left in political and financial support for WHO, calling it a “very big challenge.” Valentina echoes this sentiment, describing the U.S. exit as “very unfortunate,” noting that their expertise was missed and their absence increased pressure on other member states, particularly the EU. Still, she remains hopeful: "We showed that we were capable of achieving a good result […] and they could [re]join at a later stage.”
The Real Test: Implementation and Accountability
With the agreement adopted, the focus shifts to implementation – a word Melissa from MSF repeats often.
First, countries must translate the treaty into national policy. It is not self-executing: its principles must be reflected in domestic legislation, budgets, and operational plans. “That [implementation] is also something that we urge governments to start thinking about now. Not wait until the PABS is negotiated, [or] until the 60 countries have ratified,” urges Melissa.
Second, civil society must stay engaged – as watchdogs and partners. Groups like MSF played a critical role during negotiations. That role continues. “For the implementation, which is the real test or the second test, we need civil society organizations to ensure that governments are actually going to put the words into actions,” says Melissa.
Valentina explains that for Germany, implementation will go through the usual parliamentary procedure. Success will depend on the outcome of the PABS negotiations, political will and once again global solidarity. “That [implementation] will be crucial,” she reflects.
According to Dr Oliver Morgan, the WHO Hub for Pandemic and Epidemic Intelligence plays a central role in supporting the implementation of the Pandemic Agreement by advancing collaborative surveillance and strengthening global capacities.
Through initiatives like the Collaboratory and the Epidemic Intelligence from Open Sources (EIOS), the Hub facilitates real-time data sharing, outbreak analysis, and early warning systems across 105 countries, all grounded in a One Health approach. It also strengthens national public health agencies and leads the International Pathogen Surveillance Network (IPSN), which connects 344 active partners across 99 countries to improve genomic surveillance and promote equity in data access.
As Member States work toward finalizing the PABS annex, the Hub contributes practical expertise and helps build technical trust, including through targeted funding for low- and middle-income countries. With over 2,500 partners engaged in 2024, the WHO Hub has become a cornerstone of global collaboration and a key platform for strengthening Germany’s leadership as a multilateral actor in global health security.
Conclusion: A New Chapter, Not the Final Page
The Pandemic Agreement marks a new chapter in global health, but it is just the beginning. It signals renewed commitment to multilateralism, preparedness, and equity. Its true promise, however, will depend on what happens next: the PABS annex, and the implementation of financing, logistics, and legal frameworks.
If the global community can deliver, this agreement could be a turning point – aligning science, sovereignty, and solidarity to better protect humanity.
Ultimately, the Pandemic Agreement will be judged by one question: When the next pandemic hits, will outcomes be more equitable than in 2020?
- Will a nurse in Ghana get vaccinated at the same time as a nurse in Germany?
- Will researchers in Asia freely share a virus sample knowing their communities will have equal access to any cure?
- Will global surveillance detect a threat before it spirals out of control?
The agreement offers hope. But fulfilling that hope will take vigilance, resources, and the political courage to put global interests above narrow ones.
Related Articles


![[Translate to English:] [Translate to English:]](/fileadmin/_processed_/1/1/csm_20251215_AvianInfluenzaAI_4b4f25def7.webp)